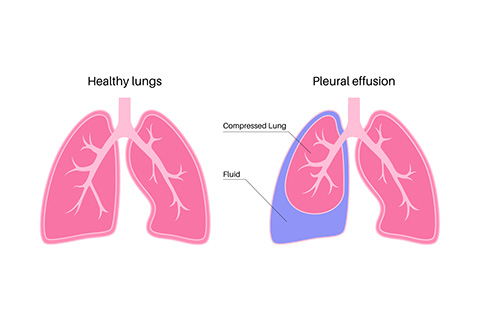
Thoracentesis is used to remove any excess fluid or air that might have built up in the pleural space, which is the thin area between the lining of your lung and the inner wall of your chest. We typically perform this procedure when we need to figure out why there's an excess of fluid, a condition known as pleural effusion, accumulating in that space. Thoracentesis may be done to treat symptoms that occur when there is too much fluid in the pleural space. When this happens, it can make it harder for your lungs to fully inflate, which can lead to symptoms like shortness of breath and discomfort or pain.
Every procedure carries risks. The risks of thoracentesis, although very low, include:
Remember to share the following information with your healthcare provider before the procedure:
To ensure your well-being and a successful procedure, please consider the following guidelines:
Your thoracentesis procedure may be conducted as an outpatient procedure, meaning you can go home the same day, or it may be part of a longer hospital stay. The specifics of the procedure can vary based on your individual condition and the methods of your healthcare provider.
Typically, you'll be asked to change into a hospital gown and remove any jewelry or other objects. Oxygen may be administered through a nasal tube or face mask, and your vital signs, such as heart rate, blood pressure, and breathing, will be monitored throughout the procedure.
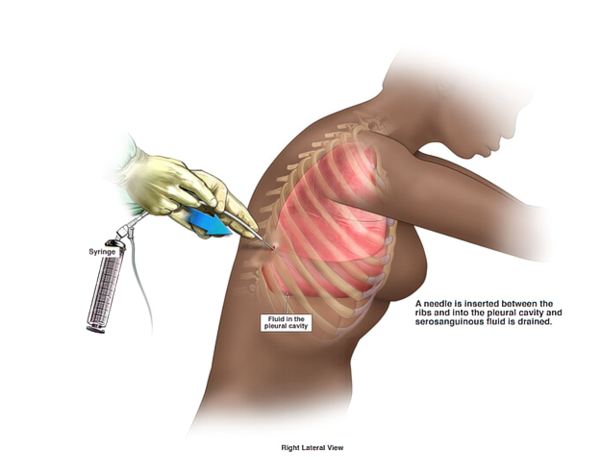
For the procedure, you'll be positioned sitting in a hospital bed with your arms resting on an over-bed table. This position helps to widen the spaces between the ribs, facilitating the insertion of the needle. If sitting is not possible, you may lie on your side at the edge of the bed.
The skin where the needle will be inserted is cleaned with an antiseptic solution, and a local anesthetic is injected to numb the area. Once numb, the healthcare provider will insert a needle between the ribs in your back. You may feel some pressure at this point as fluid is slowly withdrawn into the needle.
During the procedure, you'll be asked to remain still and may be instructed to breathe out deeply or hold your breath at certain times. If a large amount of fluid is present, tubing may be attached to the needle to allow for more fluid to drain into a bottle or bag. In some cases, a flexible tube or catheter may replace the needle and remain attached for a day or two, requiring a hospital stay until its removal.
After sufficient fluid has been removed, the needle is taken out, and a bandage or dressing is applied to the area. The fluid samples collected may be sent to a lab for further analysis.
Finally, a chest X-ray may be taken immediately after the procedure to ensure your lungs are in good condition.
After the procedure, we will closely monitor your vital signs and ensure that there is no bleeding or other fluid at the puncture site.
Following the instructions provided by your healthcare provider, you can generally resume your normal diet and activities. However, it may be necessary to avoid strenuous physical activity for a few days to allow for proper healing.
It is important to reach out to your healthcare provider immediately if you experience any complications. These may include symptoms such as fever, redness or swelling at the needle site, shortness of breath, or chest pain. Your health and well-being are Redwood Pulmonary’s top priorities, and we are here to address any concerns or issues that may arise.
To request more information, please call (650) 367-5636 or contact us online today!
Redwood Pulmonary Medical Associates
170 Alameda de las Pulgas
Redwood City, CA 94062
Phone:
(650) 367-5636
Get Directions